Table of Contents
Introduction
- Mineral trioxide aggregate (MTA) is a dental material with biocompatibility properties for oral and dental tissue.
- MTA is a hydrophilic and biocompatible endodontic cement capable of stimulating healing and osteogenesis (bone formation).
- MTA is used for creating apical plugs during apexification, repairing root perforation during root canal therapy, and treating internal root resorption.
Types of MTA
- There are two types of MTA: grey and white.
- They differ mainly in their content of iron, aluminium, and magnesium oxide.
- The difference between the grey and white MTA is the presence of iron in the grey MTA, which makes the tetra-calcium-alumina-ferrite.
- Grey MTA has large particles, a longer setting time, and greater compressive strength
- while white MTA has smaller particles with a narrower size distribution, a longer setting time, and less compressive strength.
GREY MTA | WHITE MTA |
FeO – present | FeO replaced with MgO |
FeO – Black | MgO – White (Hue matched with the colour of the tooth) |
Composition of MTA
MTA is a mechanical mixture of 3 powder ingredients:
- Portland cement (75%)
- Bismuth oxide (20%)
- Gypsum (5%)
Composition:
- tricalcium silicate, 66.1%
- dicalcium silicate 8.4%
- tricalcium aluminate, 2%
- bismuth oxide.14%
- calcium oxide, 8%
- silicon oxide 0.5%
- aluminium oxide, 1%
Bismuth is added for radiopacity
Its composition is said to be similar to that of Portland cement, except for the absence of bismuth oxide in Portland cement. Bismuth oxide is added to improve the properties and radiopacity.
Manipulation of MTA
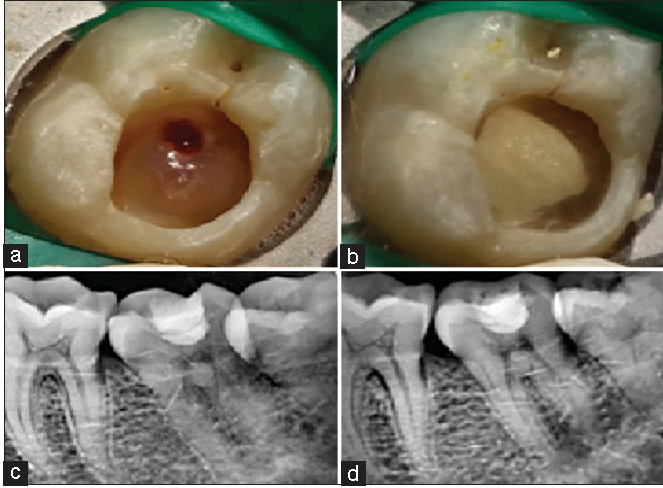
Once a decision has been made, based on clinical and radiographic evaluation, to perform MTA pulpotomy in a particular tooth, a prior written informed consent should be obtained from the parent/guardian before initiating the procedure. After the informed consent is obtained, local anesthesia is administered prior to isolation. Hereafter, the procedure to be followed, as described by Maroto et al, is as follows:
Complete isolation with rubber dam:
any endodontic procedure should be carried out under strict isolation using rubber dam, and in cases where this is not possible, pulpotomy should not be performed. The choice of isolation technique, that is, quadrant or single tooth isolation, is subjective in nature. However, quadrant isolation is preferred, if attainable, to facilitate crown preparation under rubber dam.Preparation of the molar and fitting of an SSC: Several authors have described crown preparation of a pulpotomized tooth at a later stage. However, crown preparation should precede the endodontic procedure as this would minimize the tooth structure loss and would, inevitably, be performed under local anesthesia, minimizing discomfort for the patient. Additionally, the crown fitting is done under rubber dam isolation, as has been recommended.
Removal of the carious tissue with a round bur: Excavation of dental caries is initiated with a large, slow-speed, round bur after determining the extent of the lesion before pulpal exposure.
Elimination of the roof of the pulp chamber and removal of the coronal pulp tissue: Deroofing of the pulp chamber is done with either a large, low-speed, round bur or a # 330 carbide bur. Some authors have even suggested the use of a safe-end/non-cutting end taper fissure bur for the same. After the deroofing is complete, the coronal pulp is amputated. This is done using either a large, low-speed, round bur (# 6 or # 8 round bur) or a sharp spoon excavator.
Disinfection of the pulp chamber: Some studies recommend disinfection of the pulp chamber with 3%–5% sodium hypochlorite (NaOCl) solution prior to drying of the chamber. This is known to dissolve and remove any remnant tissue, debris or dentinal chips which can lead to infection of the radicular pulp. In the 5% NaOCl, inflammation was not observed in any of the teeth. teeth had complete bridge formation (with regular or irregular tubular structure); teeth showed odontoblastic layer continuity. Thus, the cleansing action of NaOCl is non-contributory to the outcome of pulpotomy procedure. Irrigation of the pulp chamber using normal saline is adequate to remove any debris remaining in the chamber.
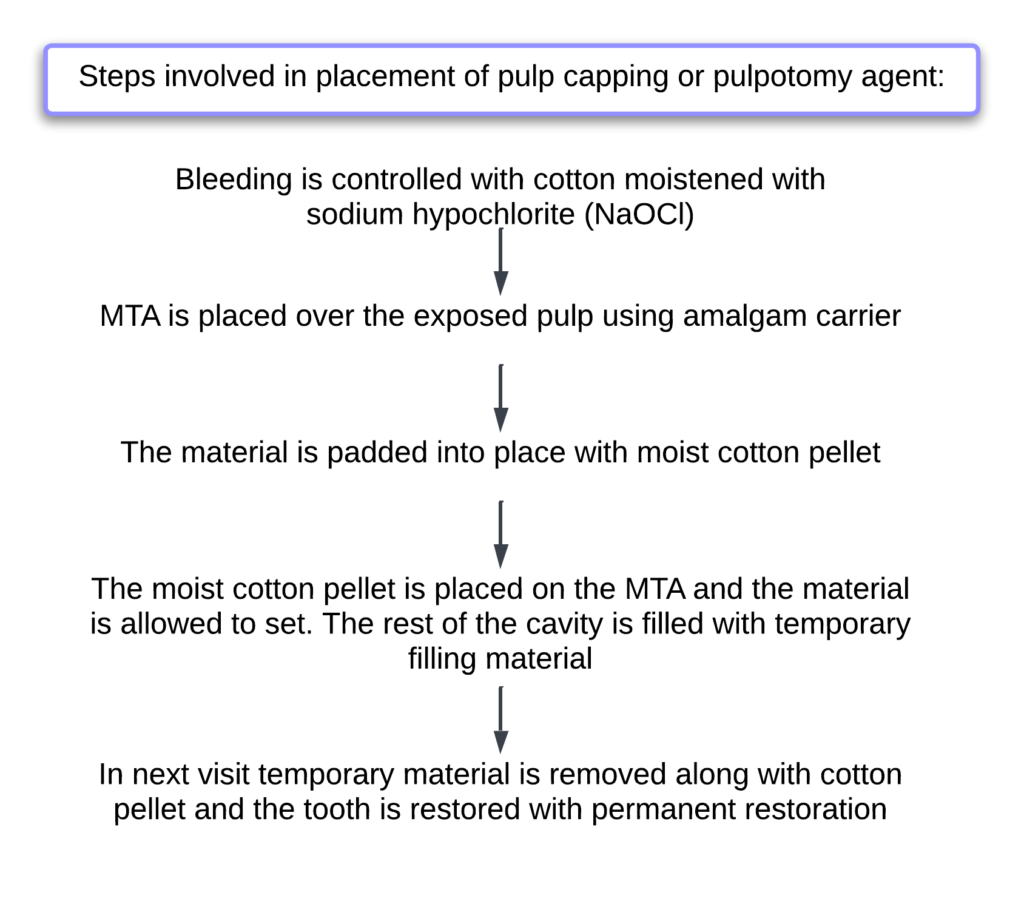
Drying and control of the pulp hemorrhage using slight pressure with a sterile cotton wool pellet: the control of bleeding should be attained within 3–5 min using a moist, sterile, cotton wool pellet. Gentle pressure should be applied against the canal orifices with this pellet. A moistened cotton pellet is recommended since the fibers from a dry cotton pellet would get incorporated in the clot and be dislodged when the pellet is removed and thus hemorrhage will resume.
At the end of the above stipulated time, on removal of the pellet, the pulp chamber should be devoid of any remnant coronal pulp tissue and hemostasis should be attained at the canal orifices. If at this stage hemorrhage still persists, one should check for remaining pulpal tissue tags and remove them immediately to attain hemostasis. To achieve this hemostasis, the use of a cotton pellet soaked with 1.25%–6% NaOCl is recommended for 1 min.
The NaOCl would dissolve any extrapulpal blood clot present between the wound surface and the medicament that interferes with healing. Shröder suggested that the presence of an extrapulpal blood clot potentiated the initial inflammatory response triggered by a pulpotomy medicament due to the chemotactic effect of the polymorphonuclear leukocytes of the fibrin in the clot.
The presence of such a clot could lead to internal resorption in the dentin adjacent to it rather than it being the effect of the medicament. If, after the removal of the moistened pellet, hemorrhage recommences, the radicular pulp is chronically inflamed, and the tooth is contraindicated for pulpotomy and pulpectomy procedure should be undertaken.Mixing of the MTA with sterile water on a glass slab following the manufacturer’s instructions: The choice of type of MTA is subjective in nature. Higher dentin bridge formation was found with gray MTA, while more necrosis and inflammatory cells were seen with white MTA in histologic evaluation, although the overall success was similar with both the materials. This difference in the two materials was attributed to tetracalciumaluminoferrite content in the material.
MTA should be mixed with sterile water as per the manufacturer’s recommendation on a clean sterile glass slab and a spatula. The final mix should have a wet, sand-like consistency.
Pressing the MTA to the walls and floor of the pulp chamber with a cotton wool pellet moistened in sterile water: Once the MTA is mixed, the cotton pellet, placed within the pulp chamber, should be removed and the MTA mix carried into it using an excavator, a retrograde amalgam or a Dovgan carrier. The increments of MTA should be compacted against the floor and walls of the chamber using a cotton pellet moistened with sterile water.The thickness of the compacted bulk of material should be 3–4 mm and should cover all of the root canal orifices and the floor. No voids should be seen. It is advisable to make a radiograph at this stage to check for adequate thickness of the MTA layer and proper compaction of the material.
Filling the pulp chamber with a glass ionomer cement: After verifying the acceptability of the MTA layer, the remainder of the pulp chamber should be restored with glass ionomer cement immediately.This concept of immediate restoration with glass ionomer cement is supported by some authors, while others state that the MTA should be covered by a moist cotton pellet followed by temporization and the patient be recalled after 24 h to remove the pellet and fill the chamber with glass ionomer cement.However, this is not necessary with the newer MTA material available in the market that has a shorter setting time than traditional ProRoot MTA or Portland cement.
Cementation of the stainless steel crown (SSC) using glass ionomer luting cement: After the pulp chamber is restored with glass ionomer cement, the predetermined and fitted SSC should be cemented with glass ionomer luting cement. Several other definitive restorations have been carried out in various studies, including amalgam restorations; however, SSCs have been found to be the most successful definitive restoration. Well-adapted SSCs eliminate the chances of procedural failure due to fracture of restoration or microleakage. After cementation, the excess glass ionomer cement should be removed and the proximal contacts be flossed using knotted floss. Randall has recommended the use of resin-modified glass ionomer cements for cementation of the crown.
Oral hygiene instructions and regular follow-up: The patient and parent should be given proper oral hygiene maintenance instructions, since in most cases, discomfort or pain reported by the patient is due to lack of brushing that area. Patients should be asked to maintain the shiny metallic appearance of the SSC. Further, the patient should be followed up on a regular basis with recall scheduled every 6 months or as part of the individual patient’s routine periodic examination.
setting mechanism of MTA
Hydration of MTA
The chemical reaction that leads to the formation of hydrophilic cement is called “hydration.”. Components of MTA cement are partially soluble in water. Soluble components react at different speeds and rates; heat occurs during the reaction, and new products form. The resulting new products cause the setting of MTA cement and provide bonding to each other in the content of the components
hydration reaction is divided into different steps,
- mixing process
- sleep process
- setting process
- cooling process
- condensation process
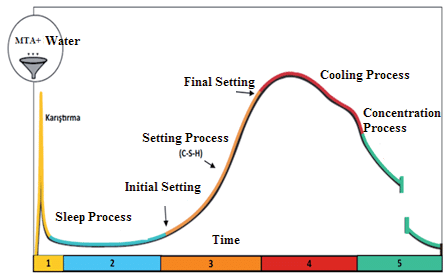
setting Mixing Process
In this process, aluminate and gypsum (CaSO4∙4H2O) dissolve in water and react within a few minutes. rapid dissolution of gypsum added to cement, aluminates dissociated from cement forms a gel-like layer around the powder particles by reacting with water. This gellike layer prevents the quick reaction of aluminates and, therefore, rapid setting of cementSleep Process –
During this process, cement can be transported, placed or processed. The duration might vary with chemical additives. Rate of heat generation remains almost constant. However, reaction still continues. Cement components dissolve and saturate with water calcium in the cement (Ca2+) and hydroxyl (OH-) ions
Setting Process –
When the water of cement is oversaturated with soluble calcium ions, new hydration products begin to form.As a result of this reaction, temperature increases. It is called the beginning of setting.Once the setting starts on the surface of cement, neither the vibrator usage nor applications such as surface finishing, cannot be performed. Such interventions lead to permanent separation Such interventions lead to permanent separation
Cooling Process –
During this process, a reaction called “topochemical” occurs. Cement has become saturated in terms of components. Hydration starts at the surface of cement particles (C3S), and hydration products (C-S-H and CH) are formed at the surface. The process of cement gaining strength also begins in this period
Concentration Process –
In this period, the reaction slows down and the heat output is reduced significantly. Hydration products continue to generate and develop slowly. Cement reaches the most rigid and robust structural properties that can be gainedThe chemical reactions that occur in the hydration step of MTA cement that we have described above are as follows: As a result of the hydrolysis of calcium silicate, calcium hydroxide in the aqueous cement (CaOH) and some calcium silicate hydrate (3CaO∙SiO2, 2CaO∙SiO2) are formed
The reaction of dicalcium silicate and tricalcium silicate is as follows:
3CaO∙SiO2+ H2O → CaO∙2SiO2∙3H2O+Ca(OH)2
2CaO∙SiO2+ H2O → 3CaO∙2SiO2∙3H2O+ Ca(OH)2
As a result of this reaction, crystal structure of hydrate is weak which forms a porous solid. This structure is called “silica gel”. Ca ions in silica gel combine with the OH ion and convert into Ca(OH)2
Once tricalcium aluminate (3CaAl2O4) is hydrated in the presence of calcium sulphate (CaSO4), it forms etringite (or sulphoaluminat calcium) with high sulphate concentration (6CaO•Al2O3•3SO3•32H2O). Etringite formation continues until all sulphate ions are used. Ettringite is converted to monosulphate once sulphate (SO2) ions are depleted.
3CaO•Al2O3•6 H2O+ H2O+ CaSO4• 2H2O → 6CaO•Al2O3•3SO3•32H2O
The resulting ettringite is disintegrated on the surface of cement particle and silicate hydrate coating is formed. After the destruction of the silicate hydrate coating, hydration can take years
It has been reported that MTA sets slowly approximately 3-4 hours in clinical conditions
Properties
- Solubility: MTA has no sign of solubility but its solubility may increase if more water is mixed. On exposure to water, MTA releases calcium hydroxide, which is responsible for its cementogenesis-inducing property.
- Compressive strength: MTA takes on average 3–4 hour to completely solidify. compressive strength of MTA within 24 hours of mixing is 40 mpa and it increase to 67.3 mpa after 21 days.
- Antibacterial and anti-fungal property: MTA has both antibacterial and anti-fungal properties; it acts as an anti-bacterial agent against enterococcus faecalis and streptococcus sanguise. act on anaerobic bacteria. as most of the flora in root canal are strict anaerobic bacteria with few facultative anaerobes.
- Tissue regeneration: it is capable of activation cementoblasts and forming cementum. MTA has property which promote the regeneration of cementum and also facilitate the regeneration of the periodontal ligament
- Radiopacity: MTA is less radio opaque than amalgam or gutta percha. Its radio opacity is 7.1 mm, equivalent to thickness of aluminium, which is sufficient to make it easy to visualise radiographically.
- Biocompatibility: Material which is not harmful or toxic to living tissue. MTA is not mutagenic and is less cytotoxic compared to EBA and IRM. MTA shows good interaction with bone-forming cells. cells remained viable and released collagen even after 72 hours with good adherence
Indication
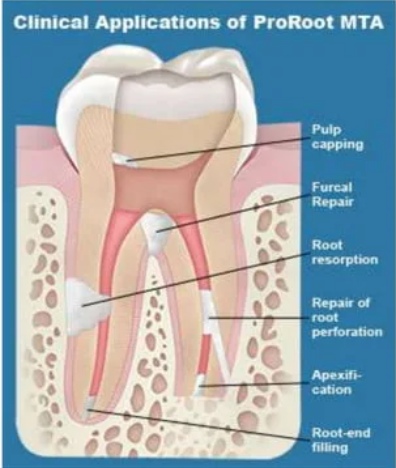
- Pulp capping:
- Pulp capping is a technique to prevent the dental pulp from necrosis after being exposed.
- MTA has been proposed as a potential medicament for capping of pulp with reversible pulpitis because of its excellent tissue compatibility.
- Although both MTA and Ca(OH)2 are used as pulp capping agent, Ca(OH)2 shows tissue reaction and inflammation or necrosis, but no such reaction are seen in pulp tissue adjacent to MTA.
- Pulpotomy:
- it is a less invasive procedure where the pulp in crown portion of the tooth is removed and the portion of the pulp which is in roots is left as it is.
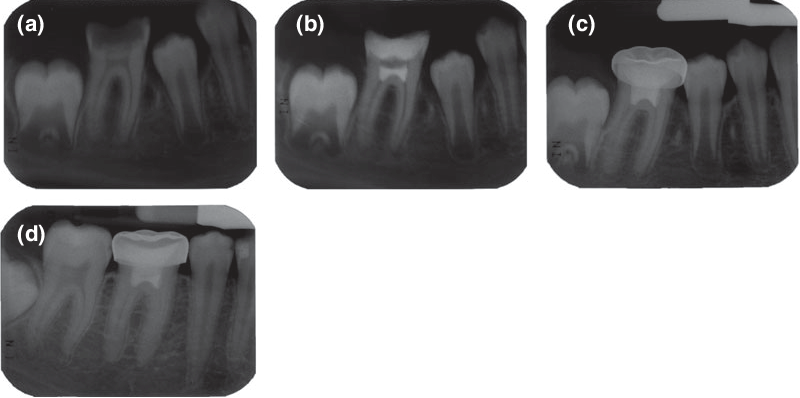
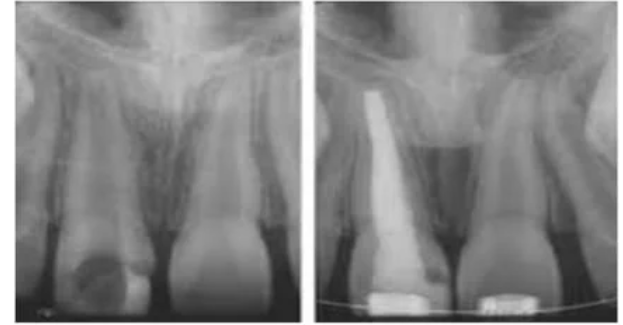
- Root end filling of immature permanent teeth
- This procedure involves surgical exposure of the root apex, root resection, and plugging the apical foramen with a suitable material, i.e., MTA, that provides a complete apical seal, is non-toxic, not resorbable, dimensionally stable, and radio-opaque.
- Step involves in root-end filling
Flap is raised under local anaesthesia, followed by ostectomy
root end resection and haemorrhage control
MTA is placed into the prepared root end cavity with a small carrier and mildly patted into place with a plugger
Since the placement of wet cotton over the setting MTA is not possible, moist environment can be created by inducing mild bleeding from adjacent tissue and bringing the blood over the MTA
The area should not be rinsed after the placement of MTA
flap is then sutured back into place
- Obturation of the canal:
- Mineral trioxide aggregate can be used to obturate the root canal of a retained primary tooth where the succedaneous permanent tooth is absent.
- To obtain coronal seal before bleaching
- MTA can be used to provide a coronal seal to a tooth that requires internal bleaching.
- A thickness of 3–4 mm of MTA placed over the condensed gutta percha in the access cavity prevents the ingress of the bleaching agent into the root portion of the tooth, i.e., the bleaching agent should remain away from the periapical area of the tooth.
- Wet cotton is placed over the MTA, and the remaining cavity is filled with temporary restoration. Later, temporary material is removed, and after the completion of bleaching, a permanent restoration is given.
- Apexification
- This is a procedure in which a calcified barrier is induced in a root with an open apex or the continued apical development of an incompletely formed root in teeth with necrotic pulp tissue.
- MTA is used to maintain the tooth in position as the root develops.
- Lateral perforation
- this happens most often during the cleaning and shaping of the canal during this procedure, the instrument perforate the canal and this perforation can be sealed with a thick mixture of MTA

- Apexogenesis:
- Apexogenesis is a dental procedure that is carried out in the case of reversible pulpitis, that is, when dental pulp is still vital or minimally inflamed.
- Apexogenesis is a procedure that preserves vital pulp tissue and allows root development in teeth with exposed and inflamed pulps. It involves removing the coronal pulp, covering it with calcium hydroxide paste, and placing a coronal restoration
Advantages of MTA
- Bio-compatibility
- Bioactive
- Hydrophilic
- Radiopacity
- Good sealing ability
- Low solubility
Disadvantages of MTA
- It has long setting time
- One of the reasons why MTA should not be implemented in a single visit is its extended setting time. (In comparison to other retrograde filling materials such as amalgam, Super-EBA, and intermediate restorative material, MTA has a longer setting time (2 h and 45 min)).
- MTA is unsuitable for most clinical applications due to its extended setting time.
Complexity of MTA
- MTA could provide significant benefits, like superior physiochemical and bioactive properties, when used as a root canal obturation material.
- MTA is an effective obturating material for retreatment; obturation is combined with root-end resection, apexification, internal resorption, dens in dente, and conventional endodontic therapy.
- Obturating with MTA enhances the prognosis and retention of the natural teeth in both conventional and complex therapies.
MTA Modification and Application:
- Despite the fact that MTA is hydrophilic material, it is never exposed to water in clinical dentistry.
- The substance has been recommended for usage as follows:
- filling material for root ends
- for repair in perforation areas
- apexification
- pulpotomy treatments
- pulp capping
- MTA has recently been introduced as a sealant for root canals.
- The generation of byproducts, that is, calcium hydroxide, and the hydrophilic nature of MTA are responsible for all of its beneficial properties. MTA interacts with a variety of environments, depending on the material application.
- When MTA is employed for repair of the perforation area, as a material for root-end filling, and, to a lesser extent, in the case of direct pulp capping (DPC), blood comes into contact with it. Blood hydrates the material and lowers MTA microhardness. Material properties and failure to set are also influenced by tissue fluids, including serum.
- The mixing and administration technique is the key problem in the clinical setting with initial MTA preparation.
- MTA is traditionally blended by manipulating the powder on a mixing pad and combining it with the powder that comes in capsule form. Alternative techniques for mixing, such as the use of an amalgamator, have also been studied.
- There is a widely held idea among researchers about cement that the surface area and initial setting time are inversely proportional. In other words, as the surface area of the powder increases, the likelihood of the particles reacting with water increases, resulting in a faster hydration process and a shorter initial setting time.
- The compressive strength of MTA was unaffected by hydroxyapatite (HA) and zinc oxide (ZnO) nanoparticles. As a result of the advantages of these nanoparticles, they can be used in cases where compressive strength is important, such as the repair of furcal perforations, pulp capping, and apexogenesis, and in cases where compressive strength is not important, such as the apical plug and as a retrograde material in surgery.
- With these advancements, MTA properties are getting better, like:
- increased setting time
- enhanced comprehensive strength
- overcome fracture
- overcome root perforation
- enhanced antibacterial activity
- enhanced regenerative ability
Modification of MTA to Overcome Fracture
- A variety of factors influence the brittleness of endodontically treated teeth.
- The use of root canal filler material to fortify the remaining tooth structure is one method of preventing vertical root fracture (VRF) in endodontically treated teeth. Despite their poor adherence to the dentinal walls of the root canal system, gutta-percha and sealers have remained the standard of care for obturating root canals in endodontics.
- MTA has been proposed as having the ability to form a tighter seal with root dentin walls than many other available materials. Ballal et al. The toughness of dentin is substantially higher in a hydrated state than in a dehydrated state.
- Another factor contributing to (OrthoMTA III)’s higher fracture resistance when compared to control and groups of ProRoot MTA is the interfacial adhesion between root canal dentin walls and MTA.
- MTA mixed with Ca, Mg-free phosphate and buffered saline had a considerable strengthening impact on the fracture resistance of structurally weak roots.
- When MTA was mixed with water and pre-treated with calcium hydroxide for 2 or 12 weeks, the strengthening effect on human roots was lost.
MTA modification to improve radiopacity and reduce tooth discoloration
- MTA, becomes unstable when it interacts with strong oxidizing agents such as sodium hypochlorite or amino acids found in dentin collagen, resulting in tooth discoloration.
- Tooth discoloration occurs when this cement is used for additional treatment techniques such as vital pulp therapy, sealing root canal perforations, and root resorptions.
- it was discovered that the addition of 5% ZnO prevented tooth discoloration and decreased the compressive strength of both MTA Angelus and ProRoot MTA cement significantly in all exposure settings.
- Zinc hydroxide creates an impenetrable barrier around tricalcium silicate, preventing hydration of the cement. Because the composition and hydration of Portland cement and MTA are similar, this negative effect may occur in MTA as well, resulting in a reduction in compressive.
Comparison of Mta and Calcium Hydroxide
PROPERTIES | Ca(OH)2 | MTA |
Hard Tissue Formation | Not much | Root end induction |
Calcific bridge | Not continuous | Continuous with dentin |
Biocompatibility | Low | High |
Degree of inflammation | Low | High |
Setting consistency | Not hard | Hard |
pH | High | High |
Solubility | Partially dissolve Permeable to fluids Soluble in periapical tissue | Less soluble Non permeable insoluble |
Application | Not easy to apply in root canal | Easy to apply in root canal through tips |
Resorption | Rate vary with density | Non-resorbable |
Apical barrier formation | Change rate/initial narrow apical width | Less/wide |
Apexification | Multiple | one |
Apical closure | Unpredictable | Good |
Patient follow up | More | Less |
Treatment | Delay | Shortened |
- Adl A., Sadat Shojaee N., Pourhatami N. (2019). Evaluation of the Dislodgement Resistance of a Newpozzolan-Based Cement (EndoSeal MTA) Compared to ProRoot MTA and Biodentine in the Presence and Absence of Blood. Scanning 2019, 3863069. 10.1155/2019/3863069 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
- Almeida L. H. S., Moraes R. R., Morgental R. D., Cava S. S., Rosa W. L. O., Rodrigues P., et al. (2018). Synthesis of Silver-Containing Calcium Aluminate Particles and Their Effects on a MTA-Based Endodontic Sealer. Dent. Mater. 34 (8), e214–e223. 10.1016/j.dental.2018.05.011 [PubMed] [CrossRef] [Google Scholar]
- Almeshari A., Elsafadi M., Almadhari R., Mahmood A., Alsubait S., Aksel H. (2021). The Additive Effect of Iloprost on the Biological Properties of Mineral Trioxide Aggregate on Mesenchymal Stem Cells. J. Dent. Sci. 17, 225–232. 10.1016/j.jds.2021.03.018 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
- Asgary S., Parirokh M., Eghbal M., Brink F. (2005). Chemical Differences between White and Gray Mineral Trioxide Aggregate. J. Endod. 31, 101–103. 10.1097/01.don.0000133156.85164.b2 [PubMed] [CrossRef] [Google Scholar]
- Ballal N. V., Rao S., Yoo J., Ginjupalli K., Toledano M., Al-Haj Husain N., et al. (2020). Fracture Resistance of Teeth Obturated with Two Different Types of Mineral Trioxide Aggregate Cements. Braz. Dent. Sci. 23 (3), 1–9. 10.14295/bds.2020.v23i3.2000 [CrossRef] [Google Scholar]
- Barczak K., Palczewska-Komsa M., Lipski M., Chlubek D., Buczkowska-Radlińska J., Baranowska-Bosiacka I. (2021). The Influence of New Silicate Cement Mineral Trioxide Aggregate (MTA Repair HP) on Metalloproteinase MMP-2 and MMP-9 Expression in Cultured THP-1 Macrophages. Int. J. Mol. Sci. 22 (1), 295. 10.3390/ijms22010295 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
- Belobrov I., Parashos P. (2011). Treatment of Tooth Discoloration after the Use of White Mineral Trioxide Aggregate. J. Endod. 37 (7), 1017–1020. 10.1016/j.joen.2011.04.003 [PubMed] [CrossRef] [Google Scholar]
- Berger T., Baratz A., Gutmann J. (2014). In Vitro investigations into the Etiology of Mineral Trioxide Tooth Staining. J. Conserv. Dent. 17 (6), 526. 10.4103/0972-0707.144584 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
- Bohns F. R., Leitune V. C. B., Garcia I. M., Genari B., Dornelles N. B., Guterres S. S., et al. (2020). Incorporation of Amoxicillin-Loaded Microspheres in Mineral Trioxide Aggregate Cement: an In Vitro Study. Restor. Dent. Endod. 45 (4), e50. 10.5395/rde.2020.45.e50 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
- Bolhari B., Meraji N., Rezazadeh Sefideh M., Pedram P. (2020). Evaluation of the Properties of Mineral Trioxide Aggregate Mixed with Zinc Oxide Exposed to Different Environmental Conditions. Bioact. Mater. 5 (3), 516–521. 10.1016/j.bioactmat.2020.04.001 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
- Boutsioukis C., Noula G., Lambrianidis T. (2008). Ex Vivo study of the Efficiency of Two Techniques for the Removal of Mineral Trioxide Aggregate Used as a Root Canal Filling Material. J. Endod. 34, 1239–1242. 10.1016/j.joen.2008.07.018 [PubMed] [CrossRef] [Google Scholar]
- Camilleri J. (2015). Mineral Trioxide Aggregate: Present and Future Developments. Endod. Top. 32 (1), 31–46. 10.1111/etp.12073 [CrossRef] [Google Scholar]
- Camilleri J., Montesin F. E., Di Silvio L., Pitt Ford T. R. (2005). The Chemical Constitution and Biocompatibility of Accelerated Portland Cement for Endodontic Use. Int. Endod. J. 38 (11), 834–842. 10.1111/j.1365-2591.2005.01028.x [PubMed] [CrossRef] [Google Scholar]
- Camilleri J. (2008). The Chemical Composition of Mineral Trioxide Aggregate. J. Conserv. Dent. 11, 141–143. 10.4103/0972-0707.48834 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
- Coomaraswamy K., Lumley P., Hofmann M. (2007). Effect of Bismuth Oxide Radioopacifier Content on the Material Properties of an Endodontic Portland Cement-Based (MTA-like) System. J. Endod. 33 (3), 295–298. 10.1016/j.joen.2006.11.018 [PubMed] [CrossRef] [Google Scholar]
- D’mello G., Moloney L. (2017). Management of Coronal Discolouration Following a Regenerative Endodontic Procedure in a Maxillary Incisor. Aust. Dent. J. 62 (1), 111–116. 10.1111/adj.12462 [PubMed] [CrossRef] [Google Scholar]
- Dianat O., Naseri M., Tabatabaei S. F. (2017). Evaluation of Properties of Mineral Trioxide Aggregate with Methyl Cellulose as Liquid. J. Dent. (Tehran) 14 (1), 7–12. [PMC free article] [PubMed] [Google Scholar]
- Duarte M. A. H., de Oliveira Demarchi A. C. C., Yamashita J. C., Kuga M. C., de Campos Fraga S. (2005). Arsenic Release provided by MTA and Portland Cement. Oral Surg. Oral Med. Oral Pathology, Oral Radiology, Endodontology 99 (5), 648–650. 10.1016/j.tripleo.2004.09.015 [PubMed] [CrossRef] [Google Scholar]
- Eskandarinezhad M., Ghodrati M., Pournaghi Azar F., Jafari F., Samadi Pakchin P., Abdollahi A. A., et al. (2020). Effect of Incorporating Hydroxyapatite and Zinc Oxide Nanoparticles on the Compressive Strength of White Mineral Trioxide Aggregate. J. Dent. (Shiraz) 21 (4), 300–306. 10.30476/DENTJODS.2020.82963.1034 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
- Formosa L. M., Mallia B., Camilleri J. (2013). A Quantitative Method for Determining the Antiwashout Characteristics of Cement-Based Dental Materials Including Mineral Trioxide Aggregate. Int. Endod. J. 46 (2), 179–186. 10.1111/j.1365-2591.2012.02108.x [PubMed] [CrossRef] [Google Scholar]
- Fridland M., Rosado R. (2003). Mineral Trioxide Aggregate (MTA) Solubility and Porosity with Different Water-To-Powder Ratios. J. Endod. 29 (12), 814–817. 10.1097/00004770-200312000-00007 [PubMed] [CrossRef] [Google Scholar]
- Ghasemi N., Salarinasab S., Rahbarghazi R., Sedghi S., Davoudi P. (2021). Effect of Incorporation of Zeolite Containing Silver-Zinc Nanoparticles into Mineral Trioxide Aggregate on Odontogenic Activity of Human Dental Pulp Stem Cells. J. Dent. (Shiraz) 22 (3), 187–192. 10.30476/DENTJODS.2020.86183.1172 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
- Ha W. N., Duckmanton P., Kahler B., Walsh L. J. (2016). A Survey of Various Endodontic Procedures Related to Mineral Trioxide Aggregate Usage by Members of the Australian Society of Endodontology. Aust. Endod. J. 42 (3), 132–138. 10.1111/aej.12170 [PubMed] [CrossRef] [Google Scholar]
- Hernandez-Delgadillo R., Del Angel-Mosqueda C., Solís-Soto J. M., Munguia-Moreno S., Pineda-Aguilar N., Sánchez-Nájera R. I., et al. (2017). Antimicrobial and Antibiofilm Activities of MTA Supplemented with Bismuth Lipophilic Nanoparticles. Dent. Mater J. 36, 503–510. 10.4012/dmj.2016-259 [PubMed] [CrossRef] [Google Scholar]
- Karabucak B., Li D., Lim J., Iqbal M. (2005). Vital Pulp Therapy with Mineral Trioxide Aggregate. Dent. Traumatol. 21 (4), 240–243. 10.1111/j.1600-9657.2005.00306.x [PubMed] [CrossRef] [Google Scholar]
- Kaur M., Singh H., Dhillon J. S., Batra M., Saini M. (2017). MTA versus Biodentine: Review of Literature with a Comparative Analysis. J. Clin. Diagn Res. 11 (8), ZG01. 10.7860/JCDR/2017/25840.10374 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
- Kharouf N., Zghal J., Addiego F., Gabelout M., Jmal H., Haikel Y., et al. (2021). Tannic Acid Speeds up the Setting of Mineral Trioxide Aggregate Cements and Improves its Surface and Bulk Properties. J. Colloid Interface Sci. 589, 318–326. 10.1016/j.jcis.2020.12.115 [PubMed] [CrossRef] [Google Scholar]
- Kim H. J., Jang J. H., Kim S. Y. (2021). Investigation of Characteristics as Endodontic Sealer of Novel Experimental Elastin-like Polypeptide-Based Mineral Trioxide Aggregate. Sci. Rep. 11 (1), 1–8. 10.1038/s41598-021-90033-9 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
- Kim Y., Lee C.-Y., Kim E., Jung I.-Y. (2011). Failure of Orthograde MTA Filling: MTA Wash-Out? J. Korean Acad. Conserv. Dent. 36 (6), 510–514. 10.5395/jkacd.2011.36.6.510 [CrossRef] [Google Scholar]
- Kogan P., He J., Glickman G. N., Watanabe I. (2006). The Effects of Various Additives on Setting Properties of MTA. J. Endod. 32 (6), 569–572. 10.1016/j.joen.2005.08.006 [PubMed] [CrossRef] [Google Scholar]
- Krastl G., Allgayer N., Lenherr P., Filippi A., Taneja P., Weiger R. (2013). Tooth Discoloration Induced by Endodontic Materials: a Literature Review. Dent. Traumatol. 29 (1), 2–7. 10.1111/j.1600-9657.2012.01141.x [PubMed] [CrossRef] [Google Scholar]
- Kucukyildiz E. N., Dayi B., Altin S., Yigit O. (2021). In Vitro comparison of Physical, Chemical, and Mechanical Properties of Graphene Nanoplatelet Added Angelus Mineral Trioxide Aggregate to Pure Angelus Mineral Trioxide Aggregate and Calcium Hydroxide. Microsc. Res. Tech. 84 (5), 929–942. 10.1002/jemt.23654 [PubMed] [CrossRef] [Google Scholar]
- Lee E. (2000). A New Mineral Trioxide Aggregate Root-End Filling Technique. J. Endod. 26, 764–765. 10.1097/00004770-200012000-00027 [PubMed] [CrossRef] [Google Scholar]
- Lim M., Song M., Hong C. U., Cho Y. B. (2021). The Biocompatibility and Mineralization Potential of Mineral Trioxide Aggregate Containing Calcium Fluoride–An In Vitro Study. J. Dent. Sci. 16, 1080–1086. 10.1016/j.jds.2021.04.019 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
- Marciano M. A., Camilleri J., Lucateli R. L., Costa R. M., Matsumoto M. A., Duarte M. A. H. (2019). Physical, Chemical, and Biological Properties of White MTA with Additions of AlF3. Clin. Oral Invest 23 (1), 33–41. 10.1007/s00784-018-2383-4 [PubMed] [CrossRef] [Google Scholar]
- Mathew A. I., Lee S. C., Rossi-Fedele G., Bogen G., Nagendrababu V., Ha W. N. (2021). Comparative Evaluation of Mineral Trioxide Aggregate Obturation Using Four Different Techniques-A Laboratory Study. Materials 14 (11), 3126. 10.3390/ma14113126 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
- Możyńska J., Metlerski M., Lipski M., Nowicka A. (2017). Tooth Discoloration Induced by Different Calcium Silicate-Based Cements: A Systematic Review of In Vitro Studies. J. Endod. 43 (10), 593–1601. 10.1016/j.joen.2017.04.002 [PubMed] [CrossRef] [Google Scholar]
- Nagas E., Cehreli Z. C., Uyanik O., Vallittu P. K., Lassila L. V. J. (2016). Reinforcing Effect of Glass Fiber-Incorporated ProRoot MTA and Biodentine as Intraorifice Barriers. J. Endod. 42 (11), 1673–1676. 10.1016/j.joen.2016.08.002 [PubMed] [CrossRef] [Google Scholar]
- Naik S., Hegde A. H. (2005). Mineral Trioxide Aggregate as a Pulpotomy Agent in Primary Molars: an In Vivo Study. J. Indian Soc. Pedod. Prev. Dent. 23 (1), 13–16. 10.4103/0970-4388.16020 [PubMed] [CrossRef] [Google Scholar]
- Parirokh M., Torabinejad M. (2010). Mineral Trioxide Aggregate: A Comprehensive Literature Review-Part I: Chemical, Physical, and Antibacterial Properties. J. Endod. 36 (1), 16–27. 10.1016/j.joen.2009.09.006 [PubMed] [CrossRef] [Google Scholar]
- Parirokh M., Torabinejad M. (2010). Mineral Trioxide Aggregate: A Comprehensive Literature Review-Part III: Clinical Applications, Drawbacks, and Mechanism of Action. J. Endod. 36 (3), 400–413. 10.1016/j.joen.2009.09.009 [PubMed] [CrossRef] [Google Scholar]
- Peng T.-Y., Chen M.-S., Chen Y.-Y., Chen Y.-J., Chen C.-Y., Fang A., et al. (2021). Impact of Zr-Doped Bi2O3 Radiopacifier by Spray Pyrolysis on Mineral Trioxide Aggregate. Materials 14 (2), 453. 10.3390/ma14020453 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
- Saghiri M. A., Kazerani H., Morgano S. M., Gutmann J. L. (2020). Evaluation of Mechanical Activation and Chemical Synthesis for Particle Size Modification of White Mineral Trioxide Aggregate. Eur. Endod. J. 5 (2), 128–133. 10.14744/eej.2020.84803 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
- Salem-Milani A., Ghasemi S., Rahimi S., Ardalan-Abdollahi A., Asghari-Jafarabadi M. (2017). The Discoloration Effect of White Mineral Trioxide Aggregate (WMTA), Calcium Enriched Mixture (CEM), and Portland Cement (PC) on Human Teeth. J. Clin. Exp. Dent. 9 (12), e1397. 10.4317/jced.54075 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
- Shin J.-H., Ryu J. J., Lee S.-H. (2021). Antimicrobial Activity and Biocompatibility of the Mixture of Mineral Trioxide Aggregate and Nitric Oxide-Releasing Compound. J. Dent. Sci. 16 (1), 29–36. 10.1016/j.jds.2020.07.018 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
- Siboni F., Taddei P., Zamparini F., Prati C., Gandolfi M. G. (2017). Properties of BioRoot RCS, a Tricalcium Silicate Endodontic Sealer Modified with Povidone and Polycarboxylate. Int. Endod. J. 50, e120–e136. 10.1111/iej.12856 [PubMed] [CrossRef] [Google Scholar]
- Tabari M., Seyed Majidi M., Hamzeh M., Ghoreishi S. (2020). Biocompatibility of Mineral Trioxide Aggregate Mixed with Different Accelerators: an Animal Study. J. Dent. (Shiraz) 21 (1), 48–55. 10.30476/DENTJODS.2019.77826.0 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
- Tawil P. Z., Duggan D. J., Galicia J. C. (2015). MTA: a Clinical Review. Compend. continuing Educ. Dent. (Jamesburg, N. J. 36 (4), 247. [PMC free article] [PubMed] [Google Scholar]
- Tien N., Lee J.-J., Jr, Lee A. K.-X., Lin Y.-H., Chen J.-X., Kuo T.-Y., et al. (2021). Additive Manufacturing of Caffeic Acid-Inspired Mineral Trioxide Aggregate/Poly-ε-Caprolactone Scaffold for Regulating Vascular Induction and Osteogenic Regeneration of Dental Pulp Stem Cells. Cells 10 (11), 2911. 10.3390/cells10112911 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
- Toida Y., Kawano S., Islam R., Jiale F., Chowdhury A. A., Hoshika S., et al. (2021). Pulpal Response to Mineral Trioxide Aggregate Containing Phosphorylated Pullulan-Based Capping Material. Dent. Mater. J. 41, 126–133. 10.4012/dmj.2021-153 [PubMed] [CrossRef] [Google Scholar]
- Torabinejad M., Hong C., McDonald F., Pittford T. (1995). Physical and Chemical Properties of a New Root-End Filling Material. J. Endod. 21 (7), 349–353. 10.1016/s0099-2399(06)80967-2 [PubMed] [CrossRef] [Google Scholar]
- Zafar K., Jamal S., Ghafoor R. (2020). Bio-active Cements-Mineral Trioxide Aggregate Based Calcium Silicate Materials: a Narrative Review. J. Pak Med. Assoc. 70 (3), 497–504. 10.5455/JPMA.16942 [PubMed] [CrossRef] [Google Scholar]
- Żuk-Grajewska E., Saunders W. P., Chadwick R. G. (2021). Fracture Resistance of Human Roots Filled with Mineral Trioxide Aggregate Mixed with Phosphate-Buffered Saline, with and without Calcium Hydroxide Pre-medication. Int. Endod. J. 54 (3), 439–453. 10.1111/iej.13426 [PubMed] [CrossRef] [Google Scholar]
- Parirokh M, Torabinejad M. Mineral trioxide aggregate: a comprehensive literature review–Part I: chemical, physical, and antibacterial properties. J Endod. 2010 Jan;36(1):16–27. [PubMed] [Google Scholar]
- Parirokh M, Torabinejad M. Mineral trioxide aggregate: a comprehensive literature review–Part III: Clinical applications, drawbacks, and mechanism of action. J Endod. 2010 Mar;36(3):400–13. [PubMed] [Google Scholar]
- Tawil PZ, Trope M, Curran AE, Caplan DJ, Kirakozova A, Duggan DJ, Teixeira FB. Periapical microsurgery: an in vivo evaluation of endodontic root-end filling materials. J Endod. 2009 Mar;35(3):357–62. [PubMed] [Google Scholar]
- Faraco IM, Jr, Holland R. Response of the pulp of dogs to capping with mineral trioxide aggregate or a calcium hydroxide cement. Dent Traumatol. 2001 Aug;17(4):163–6. [PubMed] [Google Scholar]
- Duarte MA, Demarchi AC, Yamashita JC, Kuga MC, de Fraga SC. Ph and calcium ion release of 2 root-end filling materials. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;95(3):345–347. [PubMed] [Google Scholar]Dammaschke T, Gerth HU, Züchner H, Schäfer E. Chemical and physical surface and bulk material characterization of white ProRoot MTA and two Portland cements. Dent Mater. 2005 Aug;21(8):731–8. [PubMed] [Google Scholar]
- Islam I, Chng HK, Yap AU. Comparison of the physical and mechanical properties of MTA and port-land cement. J Endod. 2006 Mar;32(3):193–7. [PubMed] [Google Scholar]
- Lee SJ, Monsef M, Torabinejad M. Sealing Ability of Mineral Trioxide Aggregate for Repair of Lateral Root Perforations. Journal of Endodontics. 1993 Nov;19(11):541–544. [PubMed] [Google Scholar]
- Schmitt D, Lee J, Bogen G. Multifaceted use of ProRoot MTA root canal repair material. Pediatr Dent. 2001 Jul-Aug;23(4):326–30. [PubMed] [Google Scholar]