Table of Contents
Introduction
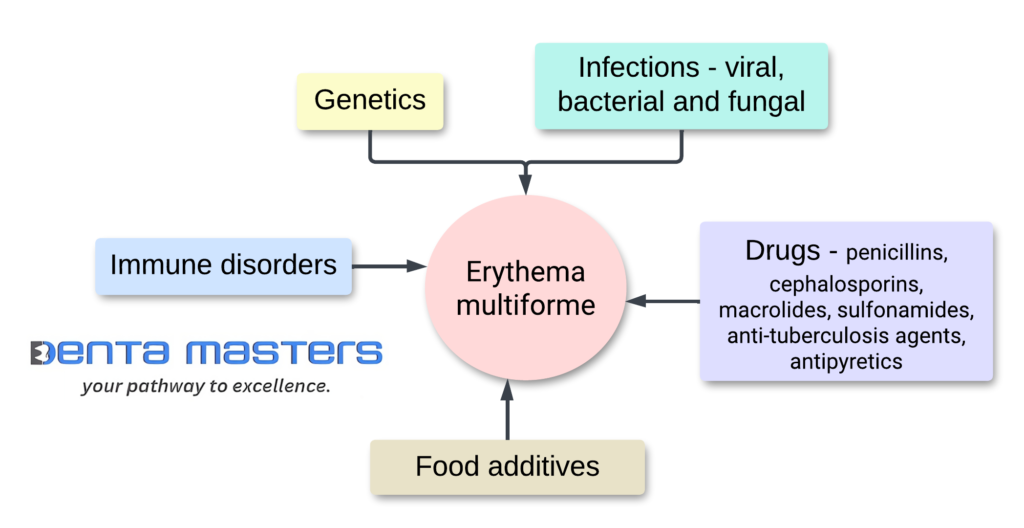
Erythema multiforme is an acute, self-healing inflammatory mucocutaneous disorder that primarily affects the skin and mucous membranes. It is triggered by various factors, such as herpes simplex virus infection, medications, and other infections. There are two types of Erythema multiforme: minor and major, with major being more severe and potentially life-threatening. The characteristic skin lesions are targetoid in appearance, while mucosal involvement is common in Erythema multiforme: major. The condition usually resolves within a few weeks. Recent research has shown that Erythema multiforme: major and Stevens-Johnson syndrome are separate conditions with similar mucosal lesions but distinct skin lesions.
Types of erythema multiforme
There are two types of erythema multiforme:
- Minor: Erythema multiforme minor is a mild form of the condition that only affects your skin and causes a rash. It’s unlikely to involve your mucous membranes (mouth, eyes, and genitals), as well as systemic symptoms such as fevers or chills
- Major: Erythema multiforme major is the most severe form of the condition. It can be life-threatening because it causes large areas of your skin to blister and peel. This type affects the mucus membranes in your mouth (oral), eyes and genitals. People usually have systemic symptoms such as fevers or joint pain.
Aetiology (study of the causes )
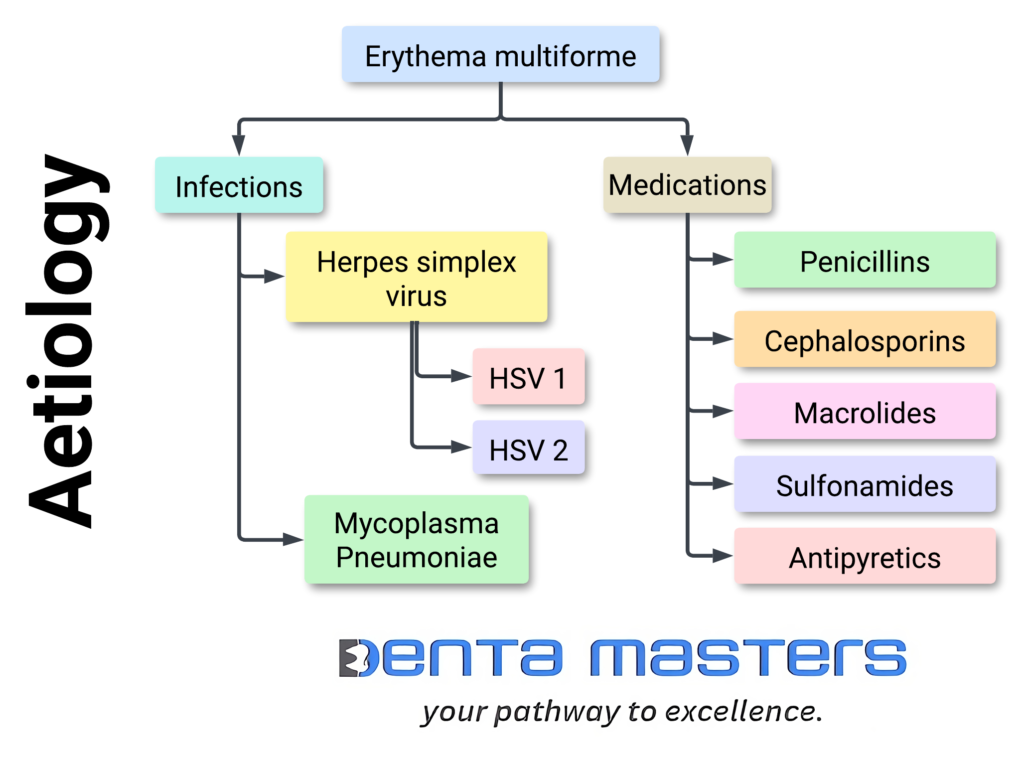
Infections
The aetiology of Erythema multiforme is most commonly Herpes simplex virus (HSV) type 1 and 2 infections and Mycoplasma pneumoniae, but many other viral, fungal, and bacterial infections have been implicated. More rarely, and in a more questionable way, vaccines have been incriminated.
Mycoplasma pneumonia infection is often listed as a trigger of erythema multiforme, however mucocutaneous manifestations associated with this infection have recently been classified as their own independent entity, Mycoplasma pneumoniae-induced rash and mucositis (MIRM).
Other infectious triggers include:
- HSV type 2
- Cytomegalovirus
- Epstein bar virus
- Influenza virus
- Vulvovaginal candidiasis
- SARS-CoV-2
- Orf
Medications
Drugs associated with Erythema multiforme include antibiotics like penicillins, cephalosporins, macrolides, sulfonamides, anti-tuberculosis agents, antipyretics, and many others. In some patients, contact with heavy metals, herbal agents, topical therapies, and poison ivy can trigger Erythema multiforme.
Medications which may trigger erythema multiforme include:
- Antibiotics (including erythromycin, nitrofurantoin, penicillins, sulfonamides, and tetracyclines)
- Anti-epileptics
- Non-steroidal anti-inflammatory drugs
- Vaccinations (most common cause in infants).
Other conditions associated with erythema multiforme (usually a persistent disease) include:
- Inflammatory bowel disease
- Hepatitis C
- Leukaemia
- lymphoma
- Solid organ cancer is a malignancy.
Epidemiology
Erythema multiforme affects less than 1% of the population. It is most common in young adults (aged 20–40 years) with a modest predominance in males; however, the disorder may involve children in 20% of cases.
Infection precipitates 90% of cases, with HSV type 1 being the predominant cause. There is no association with race.
There appears to be a genetic predisposition in people carrying the HLA-DQB1*0301 allele, which shares an even stronger association with herpes-related erythema multiforme. Multiple other alleles have been associated with its recurrent form.
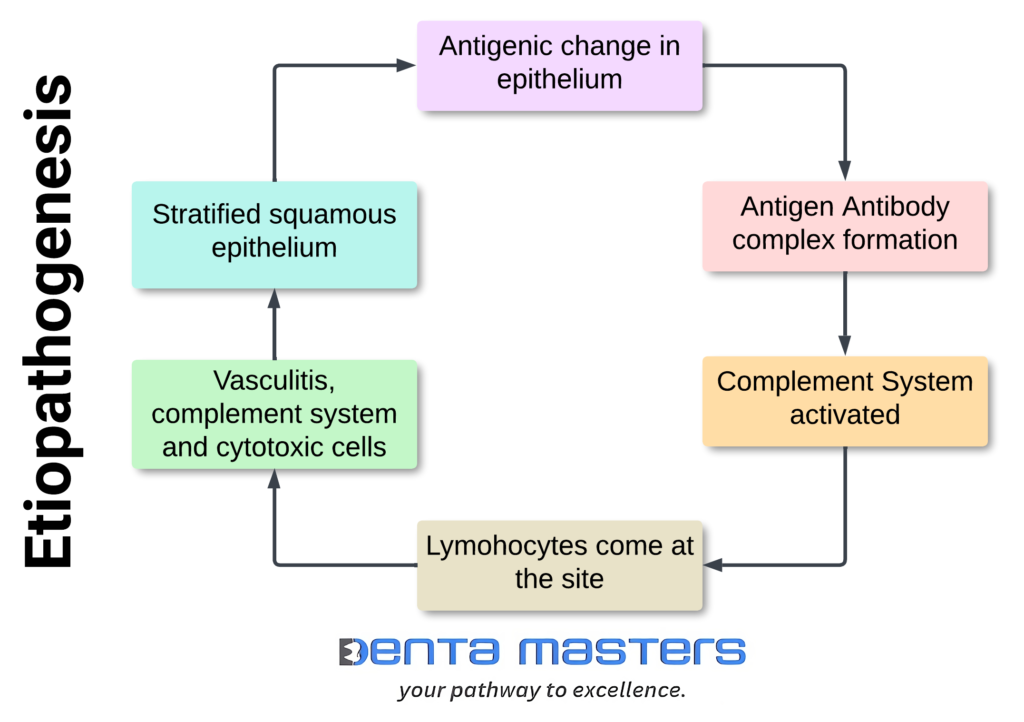
Etiopathogenesis (cause and development)
The cutaneous and mucosal lesions in Erythema multiforme are usually due to an immunological reaction to an infectious agent or drugs.The majority of Erythema multiforme patients have a history of prior herpes simplex virus (HSV) infection. Other infectious agents include bacterial (Mycoplasma pneumonia, Borreliosis), viral (Adenoviruses, Enteroviruses), and fungal infections (Coccidiodomycosis, Dermatophytes). Drugs: antibiotics (penicillin, cephalosporins, sulphonamides), non-steroidal anti-inflammatory drugs (NSAIDS), anticonvulsant drugs (phenytoin), foodstuffs (benzoates, nitrobenzene), and chemicals (perfumes) may also act as triggering factors.
Most research on the mechanism of disease has focused on the herpes-associated presentation. The herpes virus, which expresses cutaneous lymphocyte antigen (a skin-homing receptor), is phagocytosed by mononuclear cells. Engulfed viral DNA is then transferred to the epidermis and into keratinocytes. The keratinocyte layer contains viral DNA fragments that induce a cell-mediated immune response, including the production of interferon-γ, which upregulates the inflammatory process.
Sign and symptoms
The characteristic targetoid skin lesions show acral distribution with concentric colour disparity and are often accompanied by erosive lesions of the oral, genital, or ocular mucosa. Erythema multiforme major shows one or more mucous membrane involvement, in contrast to Erythema multiforme minor, which does not involve the mucosal membrane.
Clinical Features
Erythema multiforme minor may affect the feet, face, ears, palms, and back of the hands. It often presents initially on the hands or feet before moving toward the torso. Erythema multiforme major typically affects the mouth, genitals, anus, or eyes.
- Erythema multiforme lesions are usually acute in nature with mild or no prodromal symptoms. Asymmetrical erythematous maculopapular lesions eventually break and coalesce to form plaques on the skin. The target, or iris, lesion (“bull’s eye”) is the classical cutaneous lesion of Erythema multiforme. These lesions manifest as a central bulla or a pale clearing area encircled by concentric bands of edoema and erythema.
Clinical features of Erythema multiforme minor
- the initial lesion is a papule, which might enlarge and, in due course, form the characteristic targetoid lesion (an area of pale centre encircled by eythema).
- They might then progress further to form more confluent patches or annular lesions.
- The lesions in Erythema multiforme minor predominantly affect the limbs, chiefly the extensor surfaces, but sometimes they can be widespread in the body without mucous membrane involvement.
- Erythema multiforme minor presents as a bulging, rash-like lesion that is red, pink, or purple. It may look like a hive or a somewhat round bull’s-eye target. The centre of the lesion is typically darker, with lighter pink edges.
- The lesion is often circular and less than 3 cm (cm) in size, though it may be larger or smaller. The outermost circle has a well-defined border, while the centre may be a blister. The condition almost always involves the palms of the hands.
Clinical features of Erythema multiforme major
- Lesions are seen in 20% to 60% of cases and affect one or more mucous membranes.
- Oral mucosa is the most frequently affected site, and the lesions manifest initially as edoema that progresses to superficial erosions.
- Anogenital, ocular, and nasal mucosas are the other affected mucosal surfaces in Erythema multiforme major.
- People may think erythema multiforme major looks similar to erythema multiforme minor.
- However, the most significant difference in the major type is the amount of mucus and the size of the affected areas.With erythema multiforme major, at least two mucous membranes will have lesions.
- The rash is still shaped like a bull’s-eye in the major type, but it may be slightly larger, and the circles may run into each other. The lesions are more likely to blister and burst, and these areas of skin may be sore and oozing.
- Many patients report prodromal symptoms, including fatigue, malaise, myalgia, or fever. These likely represent the course of a precipitating illness rather than a true prodrome.
Cutaneous features
- Cutaneous lesions develop at the peripheries before spreading centrally.
- Distribution is usually symmetrical, with a preference for extensor surfaces.
- Lesion May be painful, pruritic, or swollen.
- Early lesions present as round, erythematous papules, which later develop into target lesions.
- Target lesions consist of three concentric rings of colour variation:
- A central, dusky area of epidermal necrosis.
- The above area is surrounded by a lighter edematous area.
- With a peripheral erythematous margin.
- Atypical lesions may be present with typical lesions. Atypical lesions are raised with poorly defined borders and/or fewer zones of colour variation.
- In severe disease, up to hundreds of lesions may be present in different developmental stages, at times making it difficult to identify characteristic lesions.
Mucosal features
- Lesions develop as blisters, which then break to reveal shallow erosions with a white overlying pseudo-membrane.
- Erythema multiforme favours oral membranes, but may also present with urogenital and, rarely, ocular lesions.
- Mucous membrane involvement can be painful and significantly limit oral intake; lesions may precede or follow cutaneous lesions.
Symptoms are expected to self-resolve within 4 weeks from onset (or up to 6 weeks in severe disease).



