Table of Contents
Introduction
Hypersensitivity reactions are considerably harmful or unpleasant. These responses result from the use of a medicinal substance. The adverse effects frequently anticipate risk from future administration and demand prevention, a particular therapy, a change in the dosing regimen, or a product withdrawal.
Types of hypersensitivity reactions
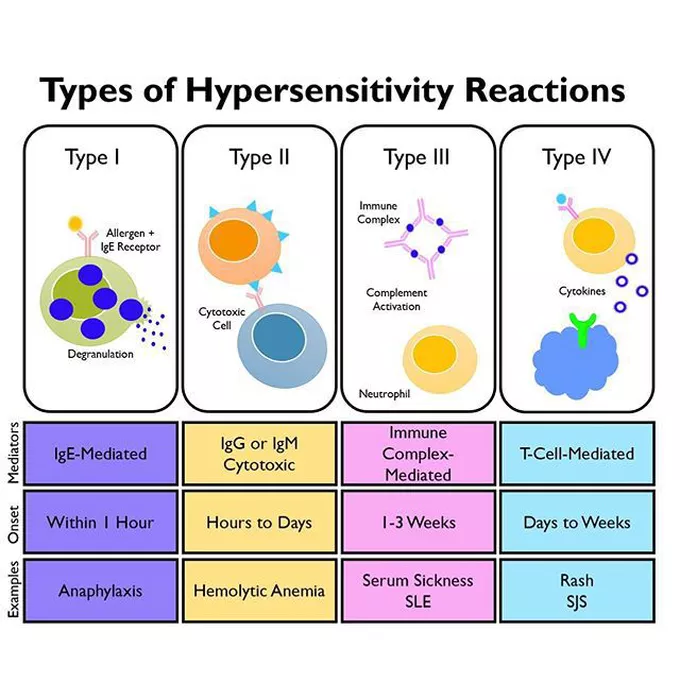
- type 1– IgE-mediated (anaphylactic). Type 1 reactions are acute (e.g., penicillin, latex, or peanut allergy) and require immediate recognition and action.
- type 2: antibody-mediated. reactions are not usually found in response to dental materials or drugs but are found in autoimmune conditions affecting the oral cavity, such as pemphigus.
- type 3: immune complex-mediated. can be seen in response to dental materials, but more commonly in response to viral infections such as recurrent herpes labialis, giving rise to erythema multiforme or Stevens-Johnson syndrome
- type 4: cell-mediated or delayed hypersensitivity or contact sensitivite reactions are reactions to dental materials that are very common. these reactions are usually seen in the oral cavity, where an amalgam or gold restoration is in direct contact with the buccal or lingual mucosa.
Type I Hypersensitivity Reactions
- Type I reactions are also called anaphylaxis.
- It is an acute, life-threatening hypersensitivity disorder defined as a generalised, rapidly evolving, multi-systemic allergic reaction.
- Without treatment, anaphylaxis is often fatal due to its rapid progression to respiratory collapse.
Pathophysiology
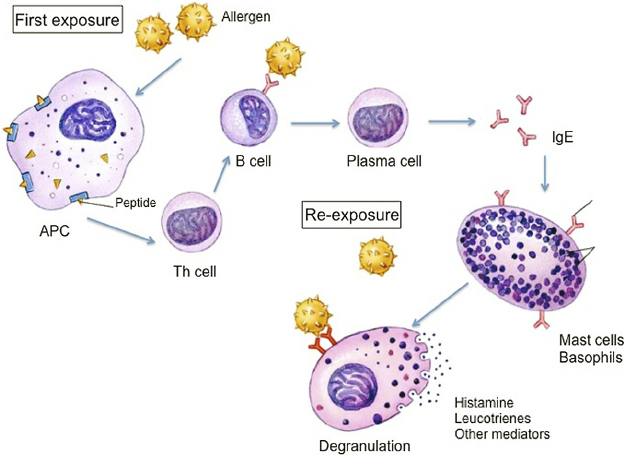
Reactions require the presence of mast cells with attached IgE.
- A patient previously exposed to a drug or other antigen has antibodies (primarily IgE) fixed to mast cells.
- When the antigen (in the form of a drug, food, or an airborne substance) is reintroduced into the body, it will react with and cross-link the cell-bound antibody.
- This causes an increase in intracellular calcium and the release of preformed mediators, including:
- histamine
- proteases
- leukotrienes and
- prostaglandins.
- Cytokines are also released, which attract eosinophils and augment the inflammatory response. These substances cause vasodilation and increased capillary permeability, ultimately leading to fluid and leukocyte accumulation in the tissues and edoema formation.
- Constriction of bronchial smooth muscle results when IgE is bound in the pulmonary region. The anaphylactic reaction may be localised, producing urticaria and angioedema, or it may result in a generalised reaction, causing anaphylactic shock.
Diagnosis
The diagnosis of anaphylaxis is a clinical diagnosis; thus, laboratory studies or other diagnostics are not necessary. Most anaphylactic deaths occur within the first hour after antigen exposure.
Consideration for anaphylaxis is appropriate in the presence of 2 or more involved systems, even in the absence of airway involvement or hypotension.
Clinical Criteria for Anaphylaxis (1 of the following with onset within minutes to hours)*
Unknown exposure to an antigen yet rapidly developing urticaria or other skin/mucosal layer symptoms associated with any one of the following:
- Respiratory symptoms (dyspnea, wheezing, stridor, hypoxemia, inability to maintain patency; persistent cough and/or throat clearing can be heralding symptoms)
- Hypotension (systolic less than 90 mm Hg or a decrease of greater than 30% from baseline)
- Signs or symptoms of end-organ dysfunction, for example, hypotonia, syncope, or incontinence
Likely exposure to an antigen and symptoms involving any 2 of the following body systems:
- Integumentary symptoms: Skin or mucosal layer (rash, pruritus, erythema, hives, swelling of the face, lips, tongue, or uvula)
- Respiratory symptoms: Dyspnea, wheeze, stridor, hypoxemia, inability to maintain patency; persistent cough and/or throat clearing can be heralding symptom
- Hypotension: Systolic less than 90 mm Hg or a decrease of greater than 30% from baseline
- Gastrointestinal symptoms: persistent, painful cramps or vomiting
Angioedema can also mimic these symptoms. A key differentiation between angioedema and anaphylaxis is urticaria; the oral symptoms and need for airway control can otherwise mimic each other. When in doubt, treat aggressively.
Kounis syndrome (allergic angina): This is a myocardial infarction or ischemia that can occur in the setting of anaphylaxis.
Treatment
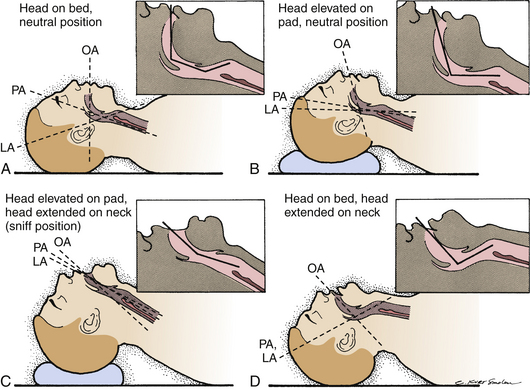
Airway
Airway management is paramount. Thoroughly examine the patient for airway patency or any indications of an impending loss of airway. Perioral edema, stridor, and angioedema are very high risk, and obtaining a definitive airway is imperative. Delay may reduce the chances of successful intubation as continued swelling occurs, increasing the risk for a surgical airway.
Decontamination
After the airway is secured, the decontamination of offending agents (if known) is the next priority to prevent continued exposure and clinical worsening. Remove any stingers, if present. Do not attempt gastric lavage in cases of ingestion, as this may not be effective and delay treatment.
Epinephrine
Epinephrine is given through intramuscular injection at a dose of 0.3 to 0.5 mL of a 1:1,000 concentration of epinephrine. Paediatric dosing is 0.01 mg/kg or 0.15 mg intramuscularly (IM) (epinephrine injection for paediatric dosage). Intramuscular delivery has proven to provide more rapid delivery and produce better outcomes than subcutaneous or intravascular delivery. Note that if intravenous (IV) epinephrine is to be given, the concentration required is 1:10,000.
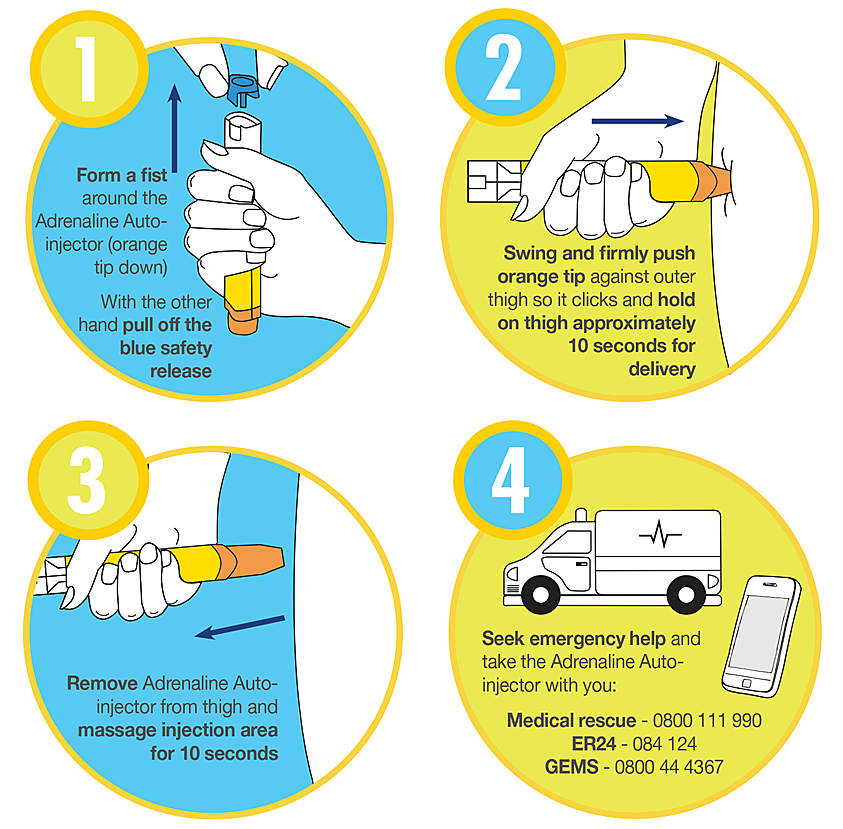
The thigh is preferred to the deltoid when possible. Repeat studies have shown that providers often wait too long before giving epinephrine; it is the treatment of choice, and the rapid benefit much outweighs the risks of withholding treatment. While most patients require only a single dose, repeat doses may be given every 5 to 10 minutes as needed until symptoms improve..
IV Fluid Resuscitation
Anaphylaxis induces a distributive shock that typically is responsive to fluid resuscitation and the above epinephrine. One to 2 L or 10 to 20 mL/kg isotonic crystalloid bolus should be given for observed hypotension. Albumin or hypertonic solutions are not indicated.
Adjunctive Therapies
Often, when anaphylaxis is diagnosed, co-treatment is initiated with steroids, antihistamines, inhaled bronchodilators, and vasopressors. Glucagon can also be used if indicated. These agents can assist in refractory initial anaphylaxis or aid in the prevention of recurrence and biphasic reactions.
Corticosteroids
Corticosteroids are given for the reduction of length or biphasic response of anaphylaxis. There is minimal literature to support this use, specifically in anaphylaxis, but it has been proven effective in reactive airway diseases. Therefore, the use, dosages, and proposed mechanism of action mimic those of airway management protocols.
Methylprednisolone (80 to 125 mg IV) or hydrocortisone (250 to 500 mg IV) are the accepted treatments during the acute phase. After which oral treatment of prednisone (40 to 60 mg daily or divided twice per day) is continued for 3 to 5 days. Again, if the source is unknown and/or there is a concern for a prolonged period prior to physician follow-up, a steroid taper of up to 2 weeks may be provided. Mineralocorticoid activity is responsible for fluid retention; in those at risk, dexamethasone and methylprednisolone are the preferred agents as they induce the least mineralocorticoid effect.
Antihistamines
Antihistamines are often routinely used; the most common is H1 blocker administration of diphenhydramine 25 to 50 mg IV/IM. While the clinical benefit is unproven in anaphylaxis, its utility is evident in more minor allergic processes. In severe cases, H1 blockers such as ranitidine (50 mg IV over 5 minutes) or cimetidine (300 mg IV) may also be used in conjunction with H-blockers, as there is evidence suggesting histamine has crossover selectivity for receptors. Note that cimetidine has multiple precautions in at-risk populations, such as renal or hepatic-impaired patients or those taking beta-blockers. While IV is the initial route during stabilisation, once the patient is stabilised, they may be switched to oral if continued therapy is desired.
Bronchodilators
Bronchodilators are useful adjuncts for patients with bronchospasm. Patients with previous histories of respiratory disease, most notably asthma, are at the highest risk. Treated with inhaled beta-agonists is the first-line treatment for wheezing: albuterol alone or as ipratropium bromide/albuterol. If there is refractory wheezing, IV magnesium is appropriate with a dosage and treatment similar to severe asthma exacerbations.
Vasopressors
Vasopressors may be substituted when a patient requires more doses of epinephrine but has unacceptable side effects from the epinephrine IV infusion (arrhythmia or chest pain). In which case there has been no clear second-line physician identified, treatment guidelines would follow those of any other patient in hypotensive shock.
Glucagon
Glucagon is the reversal agent for beta-blockers and can be used as such if needed in cases where anaphylaxis is resistant to treatment in patients with beta-blockade. Known side effects include nausea, vomiting, hypokalemia, dizziness, and hyperglycemia.
Localized Anaphylaxis –
- A localised anaphylactic reaction involving superficial blood vessels results in urticaria (hives).
- Urticaria begins with pruritus (itching) in the area where histamine and other active substances are released.
- Wheals (welts) then appear on the skin as an area of localised edoema on an erythematous base.
- These lesions can occur anywhere on the skin or mucous membranes.
- There seems to be little doubt that the oral mucosa is well endowed with mast cells and that type 1 reactions can occur in the oral cavity.
- Urticaria of the lips and the oral mucosa occurs most frequently after food ingestion by an allergic individual.
- Common food allergens include
- chocolate, nuts, shellfish, and tomatoes
- Drugs such as penicillin and aspirin may cause urticaria, and cold, heat, or even pressure may cause the reaction in susceptible individuals.
- Impression compounds, colouring agents, and preservatives, as well as ingredients of mouthwashes, may all cause local swelling or even anaphylaxis
Angioedema –
- rapid development of edematous swelling, particularly of the head and neck, sometimes accompanied by urticarial rashes.
- It occurs when blood vessels deep in the subcutaneous tissues are affected, producing a large, diffuse area of subcutaneous swelling under normal overlying skin.
- Many patients have short-term disfiguring facial swelling, but if the edoema involves the neck and extends to the larynx, it can lead to fatal respiratory failure
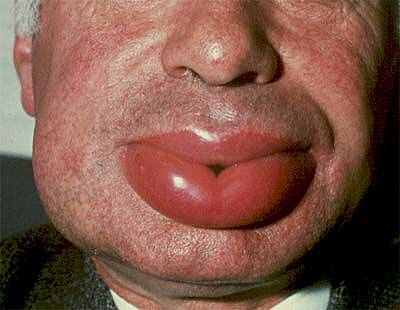
- Angioedema most commonly occurs on the lips and tongue and around the eyes It is temporary and not serious unless the posterior portion of the tongue or larynx compromises respiration.
- Respiratory distress should be treated immediately with 0.5 mL of epinephrine (1:1000) subcutaneously or, better yet, intramuscularly. This can be repeated every 10 minutes until recovery starts.
- The patient should be given oxygen, placed in a recumbent position with the lower extremities elevated unless there is a danger of shortness of breath or vomiting, given fluids intravenously, and transported to hospital immediately.
- Patients may need intubation to maintain the airway. When the immediate danger has passed, 50 mg of diphenhydramine hydrochloride (Benadryl [Pfizer, Parsippany, NJ]) should be given four times a day until the swelling diminishes.
Type II Hypersensitivity Reactions
It is an antibody-mediated immune reaction in which antibodies (IgG or IgM) are directed against cellular or extracellular matrix antigens, resulting in cellular destruction, functional loss, or tissue damage. Damage can occur via three different mechanisms:
- Antibody binding to cell surface receptors and altering its activity
- Activation of the complement pathway
- Antibody-dependent cellular cytotoxicity
Etiology
- type II hypersensitivity reaction develops in response to cell surface modifications or matrix-associated antigens generating antigenic epitopes that are regarded as foreign by the immune system.
- The most common causes include medications like penicillin, thiazides, cephalosporins, and methyldopa.
- The drug molecule either binds to the surface of cells, resulting in a neoantigen, or alters the epitopes of the existing self-antigen on the cell surface.
- This directs the immune system to recognise modified antigens as foreign, leading to the breakdown of immune tolerance and the production of antibodies directed at self-antigens.
Immune tolerance is the phenomenon by which the immune system recognizes its antigens and does not generate an antibody response against its antigens. Factors that contribute to the breakdown of tolerance promote the production of antibodies against self-antigens
Pathophysiology
In type II hypersensitivity, autoantibodies are produced (IgG and IgM) to the host cells (sensitization phase), promoting a series of pathogenic outcomes (effector phase).
The pathophysiology of type II hypersensitivity reactions can be broadly classified into three types:
- cell depletion or destruction without inflammation
- Inflammation mediated by complement or Fc receptor
- Cellular dysfunction by antibodies
The process involves a series of immune-mediated events that might take different forms
Cell Depletion or Destruction Without Inflammation:
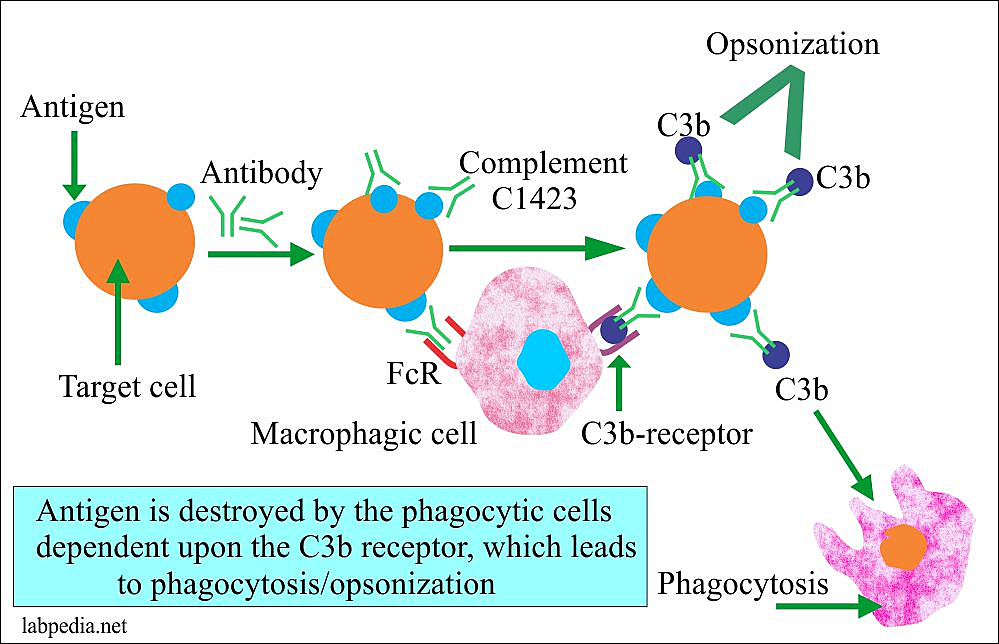
- Antibodies can bind to the target cell’s surface, particularly IgG antibodies.
- Through their Fc portion, they bind to their respective Fc receptor on the surface of macrophages and thus act as an opsonin. An opsonin is any molecule that enhances the phagocytosis of any substance.
- Thus by binding to both the target cell and the Fc receptor of the macrophage, it activates the macrophage and causes it to phagocytose the target cell.
- Antibodies can also bind to the target cell and activate the complement pathway resulting in the formation of complement component C3b.
- C3b which also acts as an opsonin and binds to the receptors on the surface of macrophages.
- This, in turn, activates the macrophages causing them to engulf the cell resulting in depletion of the cell.
Inflammation Mediated by Complement or Fc Receptor:
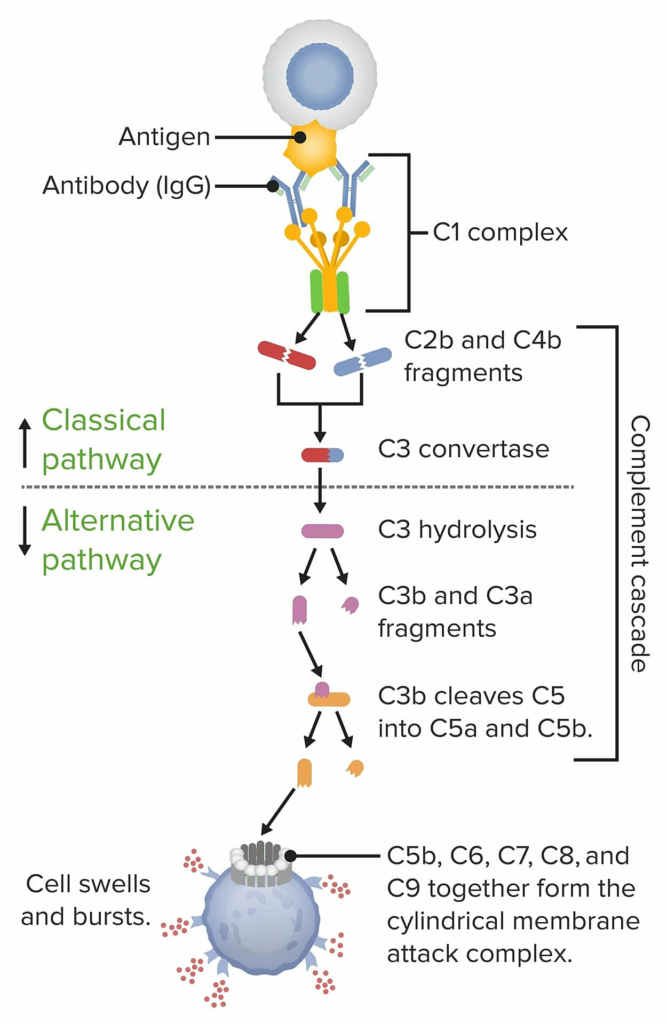
- Antibodies can activate the complement pathway by binding to self-antigens resulting in the formation of complement components C3a and C5a.
- C3a and C5a which act as chemotactic factors for neutrophils, causing the recruitment of neutrophils to the site and resulting in the activation of neutrophils.
- These neutrophils then release enzymes and reactive oxygen species, which damage the tissues.
- Antibodies against foreign antigens can also trigger complement activation and inflammation by a mechanism of molecular mimicry.
- This is the hallmark of acute rheumatic fever in which antibodies directed against streptococcal antigens structurally mimic cardiac myosin in the human heart, leading to cross-reactivity of these antibodies against bacterial and host antigens and therefore binding to the myosin and damaging the heart tissue.
Cellular Dysfunction by Antibodies
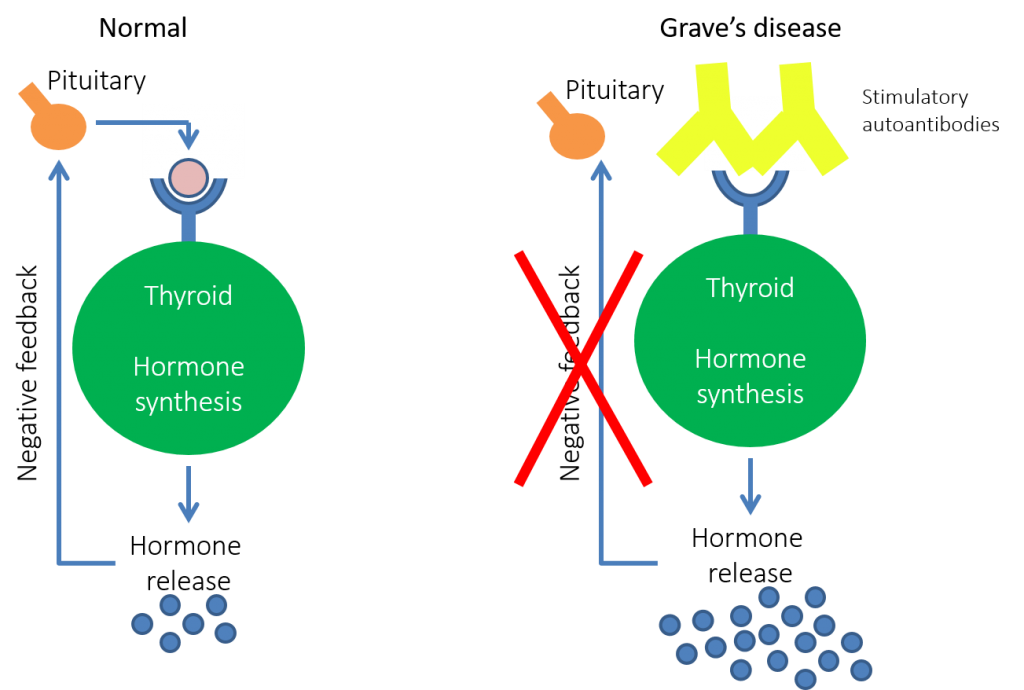
- Autoantibodies bind to the receptors on target cells, causing dysfunction without causing inflammation or destruction.
- example – in Graves disease, the autoantibodies bind to the thyrotropin receptor on thyroid follicular cells resulting in the overproduction of thyroid hormones.
- Normally, the production of thyrotropin by the pituitary is regulated by levels of thyroid hormones in the blood, but these antibodies lead to autonomous production of thyroid hormones by the follicular cells, which are not inhibited by high levels of thyroid hormones in the blood, resulting in much higher levels than cause symptoms of thyrotoxicosis
Symptoms
Signs and symptoms of type II hypersensitivity reactions include:
- thrombocytopenia and bleeding
- anemia
- bacterial and fungal infections
- neutropenia
- jaundice (in newborns)
- blistering skin
- extreme muscular fatigue
- double vision
- difficulty swallowing
Examples
Examples of type II hypersensitivity reactions include:
- rejection of an organ transplant
- Hashimoto thyroiditis
- Goodpasture syndrome
- hemolytic disease of the newborn
- myasthenia gravis
- pemphigus
- immune thrombocytopenia
- autoimmune hemolytic anemia
- autoimmune neutropenia
Diagnosis
- Doctors diagnose type II hypersensitivity reactions by confirming the presence of IgG and IgM antibodies through a blood test.
- Diagnosis is also based on your history and physical symptoms.
Treatment
- Immunosuppression is the main type of treatment for type II hypersensitivity reactions. For this, doctors often use systemic glucocorticoids to suppress the illness when it first appears or flares up.
- Intravenous immunoglobulin infusions are sometimes used to deliver human-derived antibodies to target the abnormal antibodies and neutralize them.
- Plasmapheresis, which is a procedure used to filter out a person’s antibodies and return clean blood to their body, is another possible treatment option for this type of hypersensitivity reaction.
Type III Hypersensitivity Reaction
Type III hypersensitivity reactions involve IgG antibodies binding to foreign antigens in the blood. This antibody-antigen complex gets stuck in certain locations — such as the blood vessels, skin, kidneys, or joints — and causes local damage.
Symptoms
Signs and symptoms of type III hypersensitivity reactions include:
- purpuras, which are small, non-blanching hemorrhages on the skin
- rheumatoid nodules
- a flushed rash on the face
- kidney damage
Examples
Examples of type III hypersensitivity reactions include:
- serum sickness
- rheumatoid arthritis
- systemic lupus erythematosus
- vasculitis
- glomerulonephritis
Treatment
- Treatment for type III hypersensitivity reactions involves immunosuppression, often using glucocorticoids.
- Disease-modifying antirheumatic drugs — such as methotrexate, cyclosporine, and cyclophosphamide — and biologic agents — such as TNF-blockers — are also used.
Diagnosis
- Diagnosing type III hypersensitivity reactions involves a medical history and physical exam based on your symptoms.
- There is no single test to identify the cause of this type of hypersensitivity reaction.
- Punch biopsies of vasculitis rashes can show whether or not there is local inflammation and tissue breakdown.
Type IV Hypersensitivity Reactions
Type IV hypersensitivity reactions do not involve antibodies. These are T-cell-mediated reactions that are activated by an antigen. Helper T cells recognize the antigen and send messengers that activate the immune system with killer T cells to destroy the target host.
This type of reaction occurs 48–72 hours after exposure to an antigen.
Symptoms
Symptoms of type IV hypersensitivity reactions include:
- an itchy rash
- flushed skin
- fever
- weakness
- weight loss
- skin vesicles with crust formation
- a decline in lung function
In some cases, such as with severe drug reactions, there is severe tissue damage and fluid loss that can result in hypovolemic shock. There may also be severe skin blistering that looks like a third-degree burn. In other cases, there is multiorgan involvement — particularly with the heart, lungs, kidneys, and liver.
Examples
The most common example of type IV hypersensitivity reaction is allergic contact dermatitis. The reaction that some people get to the Mantoux test, which is used to check for active tuberculosis, is also a form of type IV hypersensitivity.
There are also delayed drug reactions, including:
- Steven-Johnson syndrome (SJS)
- drug hypersensitivity syndrome
- erythema multiforme
- lichenoid drug eruptions
- morbilliform drug reactions
Diagnosis
- Doctors can diagnose these types of reactions using patch tests. With these tests, they apply a small number of potential allergens to the skin and leave them there for 2 days. If a patch of eczema forms at the site of exposure, the patch test is positive.
- A detailed medical history and physical exam are also required for an accurate diagnosis.
Treatment
- Avoiding the trigger allergen is the best form of treatment and prevention for type IV hypersensitivity reactions.
- For contact dermatitis, applying topical steroid creams can help manage skin symptoms. In the case of more severe allergic reactions, your doctor might prescribe oral corticosteroids and taper the dosage over a number of weeks.
- If SJS is present, acute care in a hospital with life saving treatment — such as fluid therapy and antibiotics — is warranted.
Okubo Y, Nochioka K, Testa MA. Nationwide Survey of Hospitalization Due to Pediatric Food-Induced Anaphylaxis in the United States. Pediatr Emerg Care. 2019 Nov;35(11):769-773. [PubMed]
Castilano A, Sternard B, Cummings ED, Shi R, Arnold T, Bahna SL. Pitfalls in anaphylaxis diagnosis and management at a university emergency department. Allergy Asthma Proc. 2018 Jul 01;39(4):316-321. [PubMed]
Akenroye AT, Ajala A, Azimi-Nekoo E, de Vos GS. Prevalence of anaphylaxis among adults admitted to critical care for severe asthma exacerbation. Emerg Med J. 2018 Oct;35(10):623-625. [PubMed]
Pattanaik D, Lieberman P, Lieberman J, Pongdee T, Keene AT. The changing face of anaphylaxis in adults and adolescents. Ann Allergy Asthma Immunol. 2018 Nov;121(5):594-597. [PubMed]
Mota I, Gaspar Â, Benito-Garcia F, Correia M, Chambel M, Morais-Almeida M. Drug-induced anaphylaxis: seven-year single-center survey. Eur Ann Allergy Clin Immunol. 2018 Sep;50(5):211-216. [PubMed]
Yue D, Ciccolini A, Avilla E, Waserman S. Food allergy and anaphylaxis. J Asthma Allergy. 2018;11:111-120. [PMC free article] [PubMed]
Parrish CP, Kim H. Food-Induced Anaphylaxis: an Update. Curr Allergy Asthma Rep. 2018 Jun 14;18(8):41. [PubMed]
Protudjer JLP, Olén O, Vetander M, Kull I, Melén E, van Hage M, Wickman M, Bergström A. Milk-Related Symptoms and Immunoglobulin E Reactivity in Swedish Children from Early Life to Adolescence. Nutrients. 2018 May 21;10(5) [PMC free article] [PubMed]
Anagnostou K. Anaphylaxis in Children: Epidemiology, Risk Factors and Management. Curr Pediatr Rev. 2018;14(3):180-186. [PubMed]
Jimenez-Rodriguez TW, Garcia-Neuer M, Alenazy LA, Castells M. Anaphylaxis in the 21st century: phenotypes, endotypes, and biomarkers. J Asthma Allergy. 2018;11:121-142. [PMC free article] [PubMed]
Valenta R, Karaulov A, Niederberger V, Gattinger P, van Hage M, Flicker S, Linhart B, Campana R, Focke-Tejkl M, Curin M, Eckl-Dorna J, Lupinek C, Resch-Marat Y, Vrtala S, Mittermann I, Garib V, Khaitov M, Valent P, Pickl WF. Molecular Aspects of Allergens and Allergy. Adv Immunol. 2018;138:195-256. [PubMed]
Graudins LV, Trubiano JA, Zubrinich CM, Elliott AS, Aung AK. Medication-related anaphylaxis treated in hospital: Agents implicated, patient outcomes, and management lessons. Pharmacoepidemiol Drug Saf. 2018 Sep;27(9):1029-1033. [PubMed]
Aun MV, Kalil J, Giavina-Bianchi P. Adults and children with anaphylaxis in the emergency room: why it is not recognized? Curr Opin Allergy Clin Immunol. 2018 Oct;18(5):377-381. [PubMed]
Navaradnam P, Suganthan N, Kumanan T, Sujanitha V, Mayorathan U. Kounis Syndrome and Multiorgan Failure Following Multiple Wasp Stings. Cureus. 2021 Apr 21;13(4):e14606. [PMC free article] [PubMed]
De Feo G, Parente R, Triggiani M. Pitfalls in anaphylaxis. Curr Opin Allergy Clin Immunol. 2018 Oct;18(5):382-386. [PubMed]
Cohen N, Capua T, Pivko D, Ben-Shoshan M, Benor S, Rimon A. Trends in the diagnosis and management of anaphylaxis in a tertiary care pediatric emergency department. Ann Allergy Asthma Immunol. 2018 Sep;121(3):348-352. [PubMed]
Gallagher JL, Rivera RD, Van Shepard K, Roushan T, Ahsan G, Ahamed SI, Chiu A, Jurken M, Simpson PM, Nugent M, Gobin KS, Wen CKF, Eldredge CE. Life-Threatening Allergies: Using a Patient-Engaged Approach. Telemed J E Health. 2019 Apr;25(4):319-325. [PubMed]
Jang HY, Ha DH, Rah SY, Lee DH, Lee SM, Park BH. Sirtuin 6 is a negative regulator of FcεRI signaling and anaphylactic responses. J Allergy Clin Immunol. 2022 Jan;149(1):156-167.e7. [PubMed]
Lindor RA, McMahon EM, Wood JP, Sadosty AT, Boie ET, Campbell RL. Anaphylaxis-related Malpractice Lawsuits. West J Emerg Med. 2018 Jul;19(4):693-700. [PMC free article] [PubMed]
Fineman SM. Optimal treatment of anaphylaxis: antihistamines versus epinephrine. Postgrad Med. 2014 Jul;126(4):73-81. [PubMed]
Leatherman BD. Anaphylaxis in the allergy practice. Int Forum Allergy Rhinol. 2014 Sep;4 Suppl 2:S60-5. [PubMed]
Rubin T, Clayton J, Adams D, Jou H, Vohra S. Systematic review of outcome measures in trials of pediatric anaphylaxis treatment. BMC Pediatr. 2014 Jun 20;14:158. [PMC free article] [PubMed]